Tips For Identifying If Your Baby Has Psychomotor Delay

Pay attention to your child’s achievements and development. This advice is valid because the notion of psychomotor delay indicates, as a provisional diagnosis, that a child’s development during his first three years of life appears as a slow or qualitatively altered sequence for his age.
The first question we must ask ourselves is: which professional should diagnose developmental problems? If you suspect that your child has some psychomotor delay, the ideal is that you take him to a specialist, who will be more objective someone in the family.
When it comes to our children, we are likely to be less than objective and overdo or minimize some precautions. However, it is vital to know when the child, during the first three years of life, does not develop or is able to walk, play or speak, which could indicate that he has some disorder.
In any case, remember that the primary care pediatrician (PA) is the most suitable professional for tracking child development. Its role is crucial for the possibility of making an early diagnosis.
Scientific societies recommend that all children periodically undergo an examination called screening for developmental delay, this should be done during visits to the pediatrician. The exam is crucial to assess your child’s psychomotor development.
According to the notes on psychomotor delay of the Spanish Association of Pediatrics, it is necessary to distinguish the global psychomotor delay, which affects not only motor acquisition but also the rate of appearance of skills to communicate, play and solve problems appropriate to their age.
In this case, it is worth considering that persistent psychomotor delay in these early years may predict a future diagnosis of mental retardation.
At other times the delay is only evident in a specific area, such as the motor achievements of posture (most often accompanied by qualitative abnormalities in muscle tone), language, or social interaction skills.
Watch for signs
The clinical impression of psychomotor delay usually appears during the first months of life, when the disproportion between observed and expected development for age is proven.
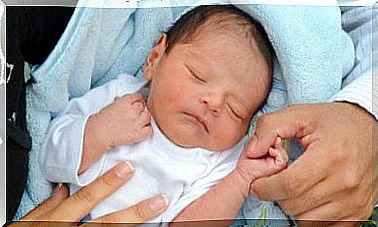
Certain children with neonatal encephalopathy show deficient behavior, and signs of neurological anomalies very early from the first days of life, according to the Spanish Association of Pediatrics.
Evidence of psychomotor delay starts in some cases from a pathological event that causes brain damage. There are early epileptic syndromes (West’s s., childhood severe myoclonic epilepsy, etc…) that lead to psychomotor delay.
It may also be that epilepsies in the early years are symptomatic of preexisting brain damage.
Many children with mild metal deficiency “completed” the first stages of psychomotor development with relative normality. Only after the second year are language delays and the relative poverty of play systems evident.
In conclusion, consultations with preschool-age children due to language, learning and social skills delay are frequent, leading to the discovery of a general psychomotor delay, followed by confirmation of mild or moderate mental retardation.
There are a few things you should be aware of during your child’s first three years of life. Here we present some of the recommendations that the Spanish Association of Pediatrics offers, and they are tips you should remember when visiting your doctor:
After birth:
- It is necessary for the physician to assess any risk factors.
- Practice neurological and behavioral examination.
- Observation of spontaneous motor skills that refer to general movements.
- Monitor hearing loss (otoacoustic emissions, audiometry by brainstem auditory evoked potentials), hypothyroidism and more frequent metabolic diseases.
2-3 months:
- Practice neurological and behavioral examination.
- Observation of motor skills and/or classic neurological examination.
- Occasionally, after hearing examination, if suspicion of hearing loss or particular risk factors persists.
- Assessment of family and social environment.
4-6 months:
- Practice neurological and behavioral examination with special attention to neck-to-trunk postural reactions, manipulation, visual behavior, and recent social interactions.
- Eye exams.
7-10 months:
- Perform neurological and behavioral examination with special attention to stable seating position, manipulation.
- Basic representative capacities, including object permanence, “appear-disappear” games.
- Imitative noise and first syllables.
12-14 months:
- Practice neurological and behavioral examination with special attention to the autonomous displacement mode, first steps. Handling with thumb-index tweezers.
- Joint attention.
- Protodeclarative gestures and first words.
18-20 months:
- Perform neurological and behavioral examination with special attention to the quality of independent walking, use of spoon and cup.
- Symbolic and fictional games, intersubjective skills.
- Lexicon evaluation, paying attention to comprehension and vocabulary. At this age, more than 50 words must be expressed.
It is useful to ask the parents to say for one minute a list of different words that they found that the child is currently emitting : if we multiply the number of words remembered by two, we will get very close to the actual number of different terms that the child uses in his/her expression .
24-36 months:
- Perform neurological and behavioral examination with special attention to the quality of walking and running.
- Basic knowledge of the body system.
- Attempt to use pencil.
- Image recognition.
- Beginning of syntaxes (subject-verb-object, some determinants and beginning of verb inflections).
- Imagination and deception play.
- Social behavior at home and at school.